Which Statement Describes a Medically Necessary Service
It means that you need a treatment to heal from your illness or injury or to save your life. Discusses incident to guidelines briefly.
Lists specific codes 97597 97598 97602 and states these codes cant be used for only a dressing change.
. Letter of Medical Necessity LMN Benefit Administration Company PO Box 550 Seattle WA 981110550 2066251800 Under Internal Revenue Service IRS rules some health care services and products are only eligible for. To some degree definitions of medical necessity vary from insurer to insurer and state to state. Under Internal Revenue Service IRS rules some health care services and products are only eligible for reimbursement from a Medical Spending Account when your doctor or other licensed health care provider certifies that they are medically necessary.
Medicare for example defines medically necessary as. A service is medically necessary if it is reasonably calculated to prevent diagnose correct cure alleviate or prevent the worsening of conditions that endanger life cause suffering or pain result in illness or injury threaten to cause or aggravate a handicap or cause physical deformity or malfunction and if there is no other equally effective although more. Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice Most health plans will not pay for healthcare services that they deem to be not medically necessary.
Which statement describes a medically necessary service. In any case in which some means of. However most definitions incorporate the idea that healthcare services must be reasonable and necessary or appropriate given a patients condition and the current standards of clinical practice.
The medical record must clearly describe the patients condition before during and after the therapy episode to support that the patient significantly benefited from ongoing therapy services and that the progress was sustainable and of practical value when measured. Using the appropriate course of treatment to fit within the patients lifestyle. Using the least radical serviceprocedure that allows for effective treatment of the patients complaint or condition.
American Dental Association ADA - Definition of Medical Necessity. The beneficiarys condition must require both the. Medicare covers ambulance services only if they are furnished to a beneficiary whose medical condition is such that other means of transportation are contraindicated irrespective if such other transportation is actually available.
Describe the MEDICAL CONDITION physical andor mental of this patient AT THE TIME OF. Describes who may perform the service physicians NPs PAs Clinical Nurse Specialists. The Intergovernmental Agreement between AHCCCS and DCS for CMDP establishes CMDP as.
Services must be necessary for treatment of the patients condition. Ambulance Transportation is medically necessary only if other means of transport are contraindicated or would be potentially harmful to. Letter of Medical Necessity.
And restoring facial configuration or function necessary for speech swallowing or chewing. Using the lease radical serviceprocedure that allows for effective treatment of the patients complaint or condition. What form is provided to a patient to indicate a service may not be covered by Medicare and the patient may be responsible for the charges.
Medical Necessity Requires that all servicesinterventions be directed at a medical problemdiagnosis and be necessary in order that the service can be billed A claims based model that requires that each serviceencounter on a stand alone basis reflects the necessity for that treatment intervention. Yet typically the decision as to whether services are medically necessary. Which statement describes a medically necessary service.
Whether your insurer deems a procedure medically necessary will determine how much of the cost if any it will cover. Treatmentmedicationequipment item in question is necessary and how you expect that it will help the patient Duration. In summary treatmentmedicationequipment item in question is medically necessary for this.
Medical necessity is a term health insurance providers use to describe whether a medical procedure is essential for your health. 143 rows Which statement describes a medically necessary service. According to the example LCD from Novitas Solutions which condition is considered a.
Medical necessity is established when the patients condition is such that use of any other method of transportation is contraindicated. Using the least radical serviceprocedure that allows for effective treatment of the patients complaint or condition. Performing a procedureservice based on cost to eliminate wasteful services.
Care is medically necessary for the purpose of controlling or eliminating infection pain and disease. The phrase medical necessity has a perfectly real urgent clinical meaning. I believe that the health insurers went too farlegally speakingwhen they took a legitimate clinical term and used it to control access to treatments.
Which statement describes a medically necessary service. What form is provided to a patient to indicate a service may not be covered by Medicare and the patient may be responsible for the charges. To be covered ambulance services must be medically necessary and reasonable.
Using the closest facility to perform a service procedure. Length of time treatmentmedicationequipment item in question is necessary not to exceed 12 months Summary. According to HealthCaregov medically necessary services are defined as health care services or supplies that are needed to diagnose or treat an illness injury condition disease or its symptoms and that meet accepted standards of medicine.
Chapter 1docx - 1 Which statement describes a medically necessary service u00a9 B Using the least radical serviceprocedure that allows for effective Chapter 1docx - 1 Which statement describes a medically. 1 10-01-03 B3-21202A A3-3114B HO-2362. Medical necessity is difficult to define with as many different interpretations as there are payers.
The service is one that a physician exercising prudent clinical judgment would provide to a patient for the purpose of preventing evaluating diagnosing or treating an illness. 1021 - Necessity for the Service Rev. Brief statement that all services must be medically necessary.
Definition of Medical Necessity The following criteria are the basis for the Plans determination that a service is medically necessary. Medical Necessity Certification Statement for Non-Emergency Ambulance Services SECTION I GENERAL INFORMATION.

Medically Necessary Defined Updated For 2022 Aginginplace Org

The Secret To Documenting For Medical Necessity Webpt

Medically Necessary Defined Updated For 2022 Aginginplace Org

Blue Cross Blue Shield International Medical Claim Form Download The Free Printable Basic Blank Medical Form Business Card Template Old Quotes Medical Claims

Medically Necessary Defined Updated For 2022 Aginginplace Org
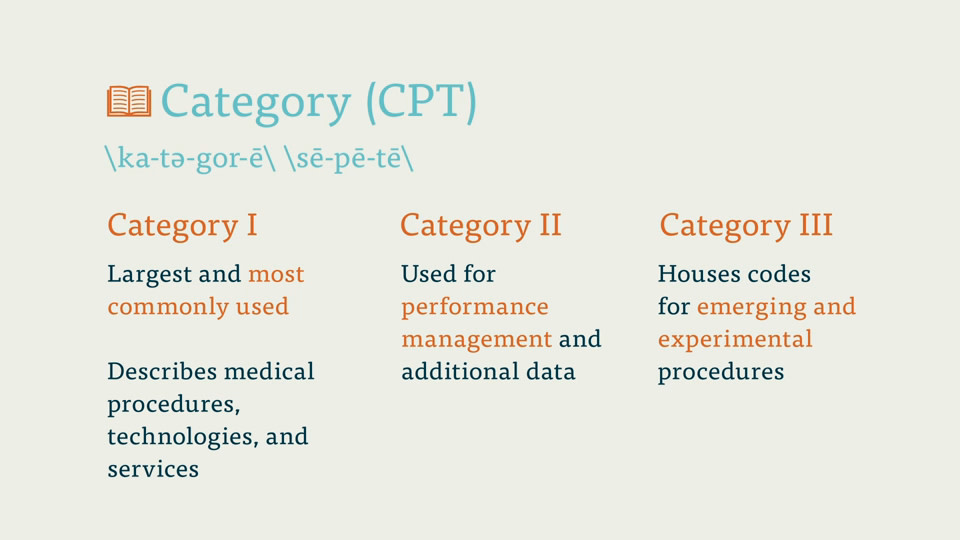
Medical Coding Vocabulary Key Terms

The 4 Cs Of Letters Of Medical Necessity Medical Special Education Resources Data Collection Special Education

Medical Necessity Versus Mdm There Is A Difference Icd10monitor
Comments
Post a Comment